
Sacral neuromodulation (SNS) is one of the treatments options practiced for overactive bladder (OAB). To be mentioned there are other neuromodulations available for OAB focused on other nerves in the body (like Tibial nerve or Pudendal nerve).
Symptoms of Overactive Bladder
Patients with OAB have a sudden, strong urge to urinate that they’re unable to ignore. This urge can cause fear of incontinence. However, the patient may or may not actually leak urine. Other symptoms include:
- Urge incontinence, or leaking urine when feeling a sudden urge to urinate
- Frequent urination, or urinating more than eight times within 24 hours
- Nocturia, or waking up more than once at night to urinate

Causes of Overactive Bladder
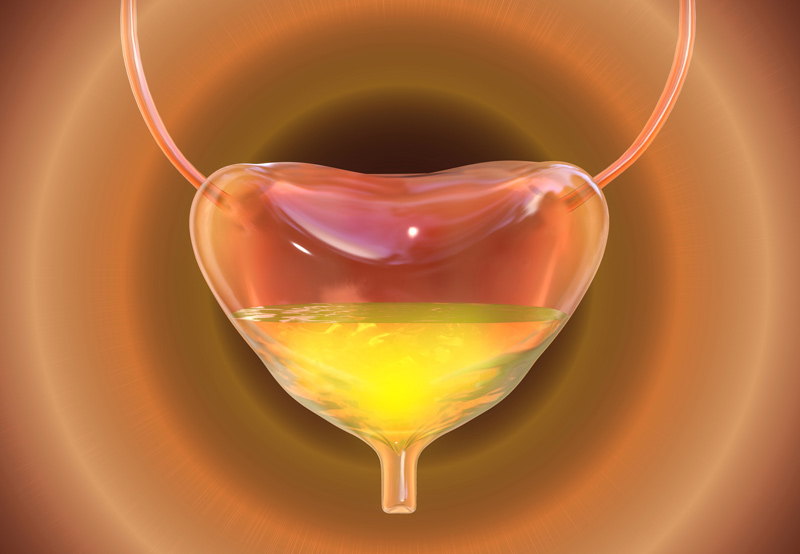
Typically, a full bladder will receive signals from the brain to squeeze the muscles and urinate. This will force urine out through the urethra, causing the sphincter to open and release urine from the body. If the bladder isn’t full, then it’s relaxed.
Patients with OAB need to urinate even if their bladder isn’t full. This can happen if the muscles in the bladder are overactive.
Risk Factors for OAB
The risk of developing OAB is heightened by the following factors:
- Changes in hormones
- Urinary tract infection (UTI)
- Pelvic muscle weaknesses or spasms
- Side effects from medication
- Neurologic disorders or damage to the nerve signals between the bladder and brain
- Conditions that affect the brain or spinal cord, such as multiple sclerosis and stroke
Diagnosing Sacral Neuromodulation
Patients experiencing symptoms of OAB should schedule a doctor’s appointment. During the appointment, the physician will review the patient’s medical history, ask about symptoms and their impact on daily life, review the patient’s current medications, and ask questions about diet and liquid intake during the day and night. The physician will also examine the abdomen, organs in the pelvis, and rectum.
The patient may need to keep a bladder diary for a few weeks to track:
- Fluid intake
- Urination
- Frequency of the need to urgently urinate
- Leakage or incontinence
A few tests that may be done to diagnose OAB include urine tests, bladder scan, cystoscopy, and urodynamic testing.
What to Expect During Sacral Neuromodulation
Depending on the patient’s unique condition, they may benefit from treatment with sacral neuromodulation.
The sacral nerve carries signals between the bladder and spinal cord, helping hold and release urine. Patients with OAB have malfunctioning nerve signals. Treatment changes the function of the sacral nerve using a bladder pacemaker. This device controls nerve signals to stop OAB symptoms.
The first part of treatment is implanting an electrical wire under the skin in the lower back. The wire will be connected to a handheld pacemaker that will send electrical pulses to the sacral nerve. The patient and physician will test the pacemaker for effectiveness. If the patient experiences an improvement in symptoms, then a permanent pacemaker will be implanted to regulate nerve rhythm.
Patients should speak to their physician to find out if they’re a good candidate for sacral neuromodulation.
Patients may also be encouraged to make certain lifestyle changes, such as limiting intake of food and drinks that irritate the bladder, such as caffeine, tea, alcohol, citrus, tomato-based foods, chocolate, spicy foods, soda, and other carbonated drinks.

